CASE REPORT | https://doi.org/10.5005/jp-journals-10001-1360 |
Occult Metastatic Papillary Thyroid Carcinoma Presenting as Submandibular Mass: An Unusual Case
1Department of ENT, Shatabdi Hospital, Mumbai, Maharashtra, India
2Department of ENT, Bhagwati Hospital, Mumbai, Maharashtra, India
3Department of ENT, RN Cooper Hospital, Mumbai, Maharashtra, India
4Department of Oral and Maxillofacial Pathology, Smile a Mile Clinic, Mumbai, Maharashtra, India
Corresponding Author: Rashu P Mittal, Department of ENT, Shatabdi Hospital, Mumbai, Maharashtra, India, Phone: +91 9892996132, e-mail: drmittal.rashu@gmail.com
How to cite this article: Mittal RP, Yadav RR, et al. Occult Metastatic Papillary Thyroid Carcinoma Presenting as Submandibular Mass: An Unusual Case. Int J Head Neck Surg 2018;9(4):131–133.
Source of support: Nil
Conflict of interest: None
ABSTRACT
Papillary carcinoma is the most common variant of thyroid cancer. A tumor less than 1 cm in size is labelled as the papillary thyroid micro-carcinoma (PTMC). Such tumors have an excellent prognosis, although a few may metastasize to cervical neck nodes. However, an infiltrated palpable neck node without evidence of thyroid disease is rare. Here, we report a case of an isolated submandibular metastasis from a clinically occult papillary thyroid carcinoma in a 40-year-old woman. The initial surgery was performed on the basis of the fine needle aspiration cytology (FNAC) report of basal cell adenoma vs cellular pleomorphic adenoma. The case was a total histopathological surprise as it was reported as a metastasis from papillary thyroid carcinoma. Subsequently total thyroidectomy and modified neck dissection was performed as per the standard surgical guidelines.
Keywords: Occult metastasis, Papillary thyroid microcarcinoma, Submandibular gland, Thyroid gland.
CASE DESCRIPTION
A 40-year-old woman presented with the right side submandibular swelling for 3 years which was gradually progressive in nature. There were no other troublesome symptoms reported by the patient such as pain or increase in size during the meal. No other significant medical history could be elicited.
Examination revealed a 3 × 3 cm size, firm, and nontender swelling in the right submandibular region. A fine needle aspiration cytology (FNAC) study showed features suggestive of basal cell adenoma vs cellular pleomorphic adenoma. The ultrasonography (USG) neck mainly revealed a 3.0 × 3.5 × 2.8 cm-sized hypoechoic lesion in the right submandibular region.
A complete submandibular mass excision was carried out on the right side and the specimen was subjected to histopathological examination. To our surprise, the biopsy report came out with a final diagnosis of papillary carcinoma favoring metastatic mass (Fig. 1).
The postoperatively USG neck was carried out which revealed a few tiny nodules in both the thyroid lobes. A USG-guided FNAC of the thyroid gland was ordered which revealed inconclusive report.
The patient subsequently underwent total thyroidectomy with the right-side modified neck dissection (MND) type III (levels I–V) along with a bilateral central compartment clearance. Complete specimen along with neck nodes was sent for histopathological examination which revealed differentiated papillary carcinoma involving the upper pole of the right lobe of thyroid with scanty foci of extrathyroidal extension and nodal metastasis (Fig. 2).
The 100 μCi neck scan was ordered a month later which showed an iodine uptake of 0.92% with no active foci (probably due to iodine interference). A large dose scan after 3 months followed with 122 μCi of I131 was given orally. No evidence of any recurrence or nodal presentation is noted in the follow-up period, till date.
DISCUSSION
A papillary variant is the most common form of thyroid cancer and commonly remains clinically silent until its incidental histological diagnosis in surgical material or at autopsy. Nodal metastases relating to papillary thyroid carcinoma commonly involve the central compartment. Submandibular nodal metastases are rare and are usually associated with extensive cervical metastases.1
Compared with other cancers, papillary carcinoma of the thyroid gland is a relatively indolent disease with a better survival rate.2 Papillary microcarcinoma is a morphological variant of papillary carcinoma, originally described in 1949 by Hazard et al.3 based on the size of the lesion. The upper limit of size to define papillary microcarcinoma is generally 10 mm. This case is unusual in the aspect that the metastasis was confined to a single site in the right submandibular space without cervical lymphadenopathy.
Patients with clinical occult thyroid papillary carcinoma may rarely present with metastatic neck nodes.4 Distant metastases from an occult papillary thyroid carcinoma are extremely rare. To our knowledge, there have been only a few reports of an isolated metastasis from an occult papillary thyroid carcinoma to the submandibular gland. The rarity of this occurrence can be appraised from the fact that only 1–4% of all head and neck tumors are malignant neoplasms of the major salivary glands.5 Metastatic tumors account for approximately 3% of malignant salivary gland neoplasms and only 10–20% of such metastatic tumors occur in the submandibular glands.5
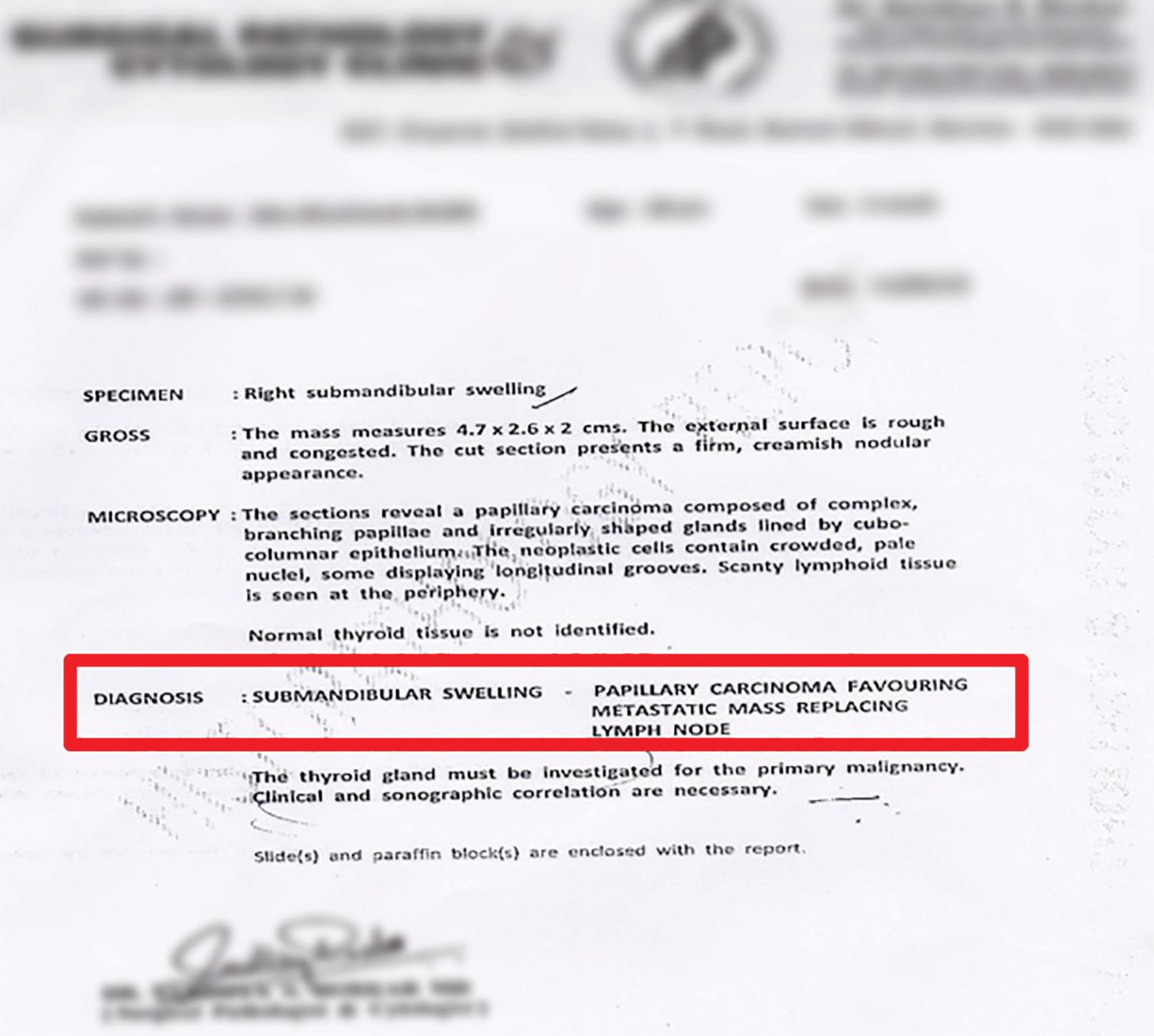
Fig. 1: Histopathology report: excised submandibular mass
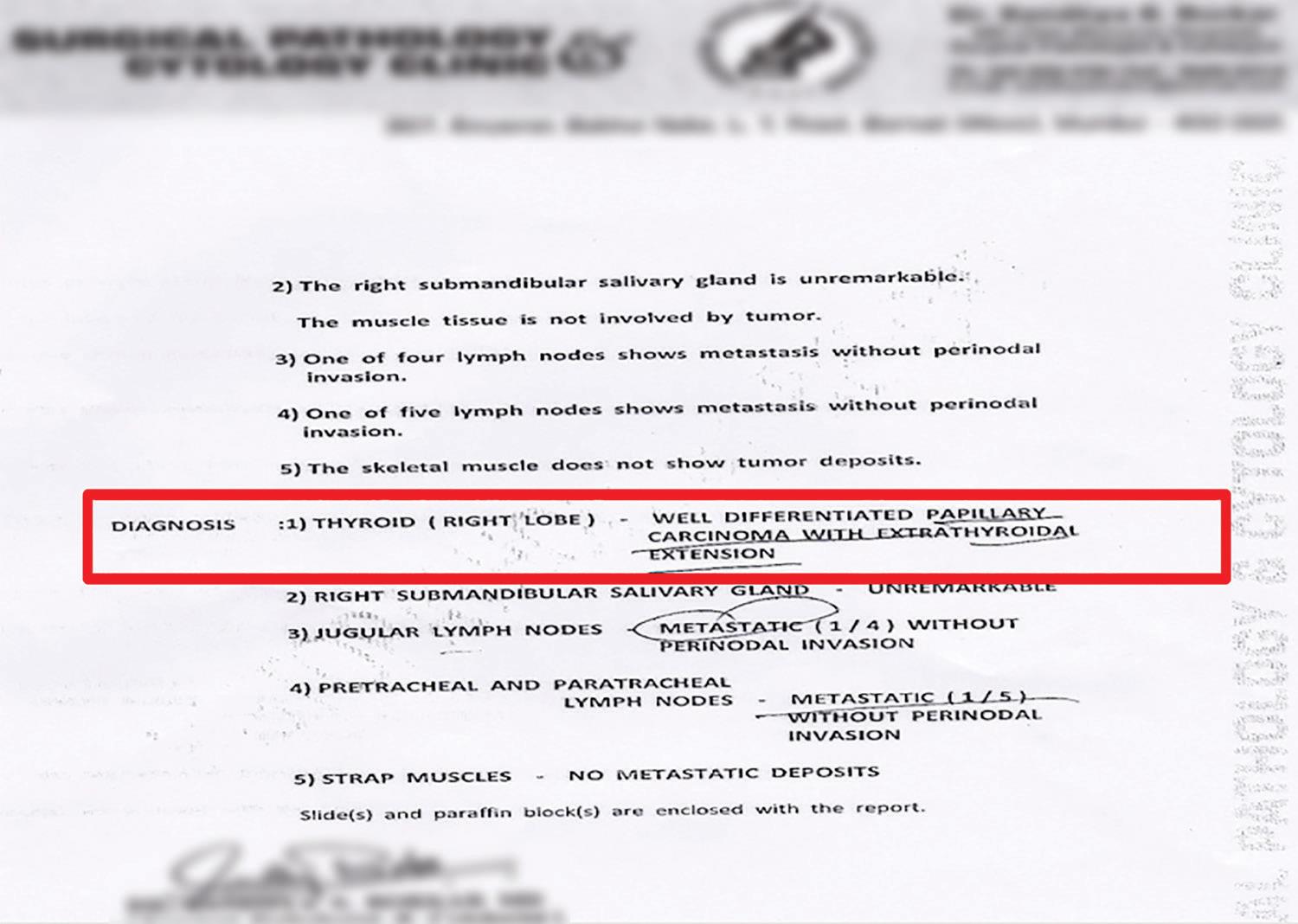
Fig. 2: Histopathology report: excised total thyroidectomy specimen along with neck nodes
Among all the salivary gland tumors, 85% occurred in the parotid gland of which 18% were malignant, 7% were in the submandibular gland of which 37% were malignant, and 8% in the major sublingual and the minor salivary glands of which 47% were malignant.6
Whereas metastases spread to the parotid gland is mainly by the lymphatic route, the majority of metastases to the submandibular gland are from a distant source namely the hematogenous route. Possibly, this difference lies in the paucity of the lymphoid tissue inside the submandibular gland, while the parotid gland may contain abundant lymphatic tissue within its capsule.7 While the extensive lymphatics surrounding the parotid gland make it susceptible to metastases from head and neck tumors, scarcity of the lymphatic tissue surrounding the submandibular gland protects it from such spread.8
Fine needle biopsy (FNB) cytology of a cervical lymph node has been proposed as a very useful procedure to discover occult thyroid carcinoma lying within the node.9 However, other studies have reported 29–43% and even 50% of non-diagnostic or false-negative results in FNB cytology of the affected lymph node. The possibility of false-negative diagnosis is even higher in the case of cystic degeneration of the lymph node metastasis10 because the classical pathologic features of PTMC, such as papillae and psammoma bodies, may be sparse or not present, and nuclear abnormalities may be the only finding.11 Therefore, negative FNB cytology results cannot safely exclude the thyroid origin of the lesion.
CONCLUSION
In conclusion, a patient with PTMC presenting as a metastatic mass with no evidence of primary thyroid tumor in thyroid imaging and inconclusive lymph node FNB cytology is reported. In such cases, thyroid malignancy should be excluded. Lymph node excision and histological examination provide the definite diagnosis.
A palpable lesion in the submandibular gland is a primitive salivary gland tumor;12 metastatic tumors are rare. This report wants to emphasize that a metastasis from an occult neoplasm must be considered whenever an unusual carcinoma in seen in a salivary gland, especially the submandibular gland.
REFERENCES
1. Noguchi S, Noguchi A, et al. Papillary carcinoma of the thyroid. I. Developing pattern of metastasis. Cancer 1970;26:1053–1060. DOI: 10.1002/1097-0142(197011)26:5<1053::AID-CNCR2820260513>3.0.CO;2-X.
2. Yousem DM, Scheff AM. Thyroid and parathyroid. In. ed. PM, Som HD. Curtin ed. Head and neck imaging,St Louis: Mosby; 1996. pp. 952–975.
3. Hazard JB, Crile GJr, et al. Non-encapsulated sclerosing tumors of the thyroid. J Clin Endocrinol 1949;9:1216–1231. DOI: 10.1210/jcem-9-11-1216.
4. Allo MD, Christianson W, et al. Not all “occult” papillary carcinomas are “minimal”. Surgery 1988;104:971–976.
5. Vaidya AM, Vaidya AM, et al. Isolated submandibular gland metastasis from oral cavity squamous cell carcinoma. Am J Otolaryngol 1999;20:172–175. DOI: 10.1016/S0196-0709(99)90067-4.
6. Eneroth CM. Salivary gland tumors in the parotid gland, submandi-bular gland, and the palate region. Cancer 1971;27:1415–1418. DOI: 10.1002/1097-0142(197106)27:6<1415::AID-CNCR2820270622>3.0.CO;2-X.
7. Feinmesser R, Lahovitzki G, et al. Metastatic carcinoma to the submandibular salivary gland. J Oral Maxillofac Surg 1982;40:592–610. DOI: 10.1016/0278-2391(82)90290-7.
8. Cain AJ, Goodland J, et al. Metachronous bilateral submandibular gland metastases from carcinoma of the breast. J Laryngol Otol 2001;115:683–684. DOI: 10.1258/0022215011908649.
9. Matsuda M, Nagumo S, et al. Occult thyroid cancer discovered by fine-needle aspiration cytology of cervical lymph node: a report of three cases. Diagn Cytopathol 1991;7:299–303. DOI: 10.1002/dc.2840070318.
10. Cunha N, Rodrigues F, et al. Thyroglobulin detection in fine-needle aspirates of cervical lymph nodes: a technique for the diagnosis of metastatic differentiated thyroid cancer. Eur J Endocrinol 2007;157:101–107. DOI: 10.1530/EJE-07-0088.
11. Monchik JM, De Petris G, et al. Occult papillary carcinoma of the thyroid presenting as a cervical cyst. Surgery 2001;129:429–432. DOI: 10.1016/S0039-6060(01)60495-1.
12. Eneroth CM. Salivary gland tumors in the parotid gland, submandi-bular gland, and the palate region. Cancer 1971;27:1415–1418. DOI: 10.1002/1097-0142(197106)27:6<1415::AID-CNCR2820270622>3.0.CO;2-X.
________________________
© The Author(s). 2018 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted use, distribution, and non-commercial reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.