CASE REPORT |
https://doi.org/10.5005/jp-journals-10001-1453 |
Recurrent Neck Abscess Secondary to Pyriform Sinus Fistula: A Diagnostic Challenge
1,2Department of Pediatric Surgery and Pediatric Urology, BLK-Max Super Speciality Hospital, New Delhi, India
3Department of Radiology, Dr. Doda's Diagnostics and Healthcare, New Delhi, India
Corresponding Author: Prashant Jain, Department of Pediatric Surgery and Pediatric Urology, BLK-Max Super Speciality Hospital, New Delhi, India, Phone: +91 9582413828, e-mail: docpedsurg@gmail.com
Pyriform sinus fistula are rare branchial anomalies which can present as recurrent suppurative neck infections. There diagnosis and management can be challenging. Ignorance about this rare entity can delay the diagnosis and can increase the challenges for surgeon to achieve recurrence free curative excision. How to cite this article: Jain P, Prasad A, Jain S. Recurrent Neck Abscess Secondary to Pyriform Sinus Fistula: A Diagnostic Challenge. Int J Head Neck Surg 2021;12(3):111-113. Source of support: Nil Conflict of interest: NoneABSTRACT
Keywords: Branchial arch anomaly, Pyriform sinus fistula, Recurrent neck abscess.
INTRODUCTION
Branchial anomalies are common cause of pediatric congenital head and neck lesions and are second in incidence to thyroglossal cyst and sinuses.1 Branchial anomalies commonly present as cyst, sinus or fistula and among these branchial sinus is the most commonly seen anomaly. Up to 95% of the branchial arch anomalies arise from the second branchial arch, while the remaining 1 to 4% originate from the 1st arch and only very few cases arise from the 3rd or the 4th arch.1,2,3 They have variable anatomy and both open into the pyriform sinus and are therefore collectively known as pyriform sinus fistula. We report a rare case of pyriform sinus fistula with recurrent neck abscess drained multiple times.
CASE DESCRIPTION
A 4-year-old girl, presented with complaint of leakage of food particles [Fig. 1] through a fistulous opening on the left lower neck. She had undergone multiple procedures for drainage of recurrent suppurative neck abscess and once excision of sinus, considering it as tubercular sinus. On examination, she had a small fistulous opening at the lower left side of the neck with purulent discharge and surrounding induration. She was already investigated in form of magnetic resonance imaging [MRI], contrast swallow studies but none of the investigations were conclusive. Repeat barium swallow done did not reveal any fistulous communication. She was then evaluated with computed tomogram [CT] scan neck with oral contrast and fortunately this time a fistulous communication could be delineated between the pyriform fossa and the external opening, confirming the diagnosis of pyriform sinus fistula [Fig. 2]. The patient was planned for the excision of fistula. Fistula could not be located on direct laryngoscopy, but after initial dissection, the tract could be easily cannulated. The tract was mobilized keeping dissection close to the tract. The tract was identified coursing in between the carotids, thereafter piercing the thyrohyoid membrane, and then cranially to open into the pyriform fossa [Fig. 3]. The tract was completely excised and the internal communication was closed. The suture line was covered with the surrounding muscle tissue, followed by layered closure. Postoperatively the child was put on nasogastric feeding for 3 days and then started on oral feeding. Histopathology report was confirmative of the branchial sinus fistula. The child is on regular follow up for the last 2 years without any recurrence.

Fig.1: Opening of previously operated sinus in left lower neck with leakage of milk
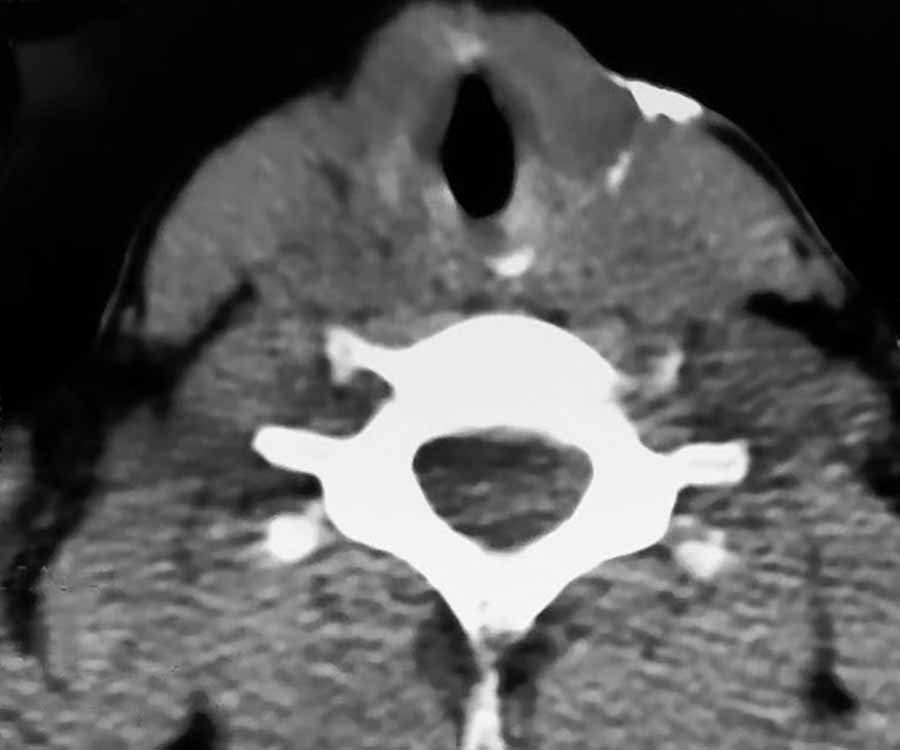
Fig. 2: CT scan demonstrating the sinus tract
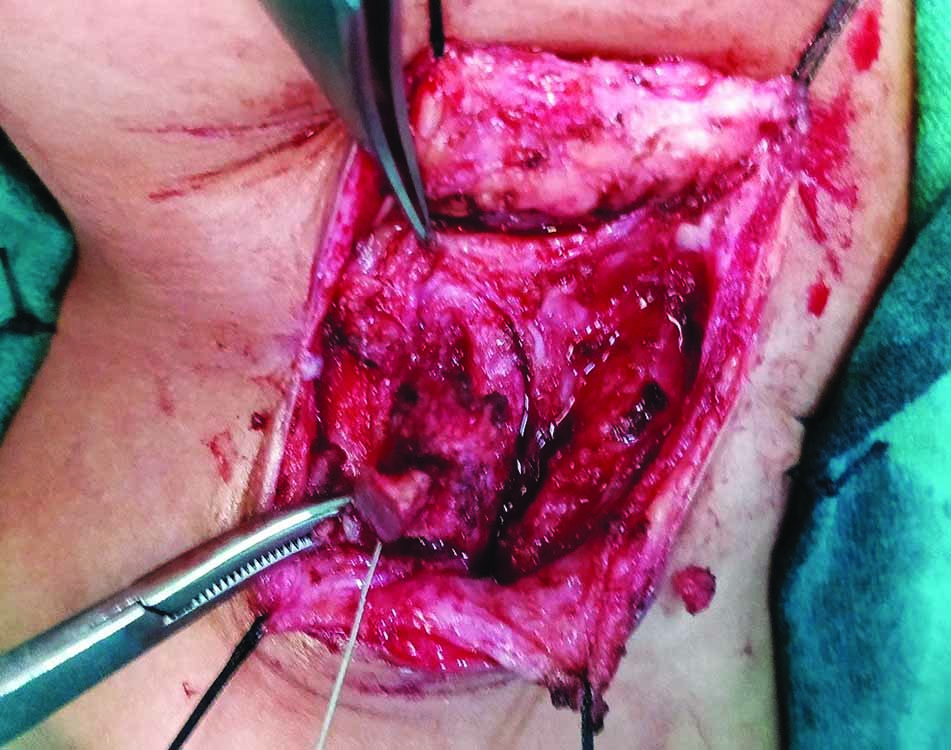
Fig. 3: Dissection of pyriform fistula piercing the thyrohoid memebrane
DISCUSSION
Branchial apparatus in humans consists of five pairs of mesodermal arches separated by four pairs of ectodermal and endodermal pouches/clefts. Branchial fistulae originate from the remnants of pouches and clefts following rupture of the interposing branchial plate.1,3,4,5,6 The 3rd branchial arch anomalies are thought to arise from the base of the pyriform fossa and passes through the thyrohyoid membrane and is located above the superior laryngeal nerve, while the 4th arch anomalies arise from the apex of the pyriform fossa and passes through the cricohyoid membrane, below the superior laryngeal nerve. Since both of these anomalies are prone to infection, it is difficult to distinguish between the two surgically. They both have similar clinical manifestations and the management is also the same, so they are collectively called as pyriform sinus fistulas.3,4,5 They can present as cysts, sinus, fistula, or abscess [subcutaneous, retropharyngeal/parapharyngeal] presenting as unilateral painful neck swelling, fever, dysphagia etc. Additionally, they may also present as an acute suppurative thyroiditis.2,3,4 They are most common in the first decade of life and predominantly occurs on the left side. A high index of suspicion is required to diagnose and manage these lesions, especially if it’s a left lower neck recurrent abscess.2
Investigations proposed include a barium swallow, and MRI or CT scan,2,7 but as observed in this case, CT scan with oral contrast had a better delineation of the fistulous tract. Our patient was operated multiple times before presenting to us. This was because the diagnosis was not confirmed and track was not demonstrated in previous investigations.
Surgical removal of the fistula and occlusion of the internal opening is the definite management.3,7 A systematic review by Nicoucar et al.4,5 reported a success rate of 85% for open neck surgical procedures and they proposed open surgical procedures in children more than 8 years and endoscopic cauterization in children under 8 years as the rate of complication was more in the latter group. Endoscopic obliteration of the sinus using chemo cauterization8 laser,9 or electrocautery10 are various minimally invasive techniques described in the literature with variable success rates. However these are small case series without long term results.3,4
Due to the variable anatomy, finding the internal opening is a challenge. Some surgeons perform laryngoscopy and localize the internal opening and inject methylene blue to delineate the tract,3 however we believe that it is difficult to locate the internal opening and also injecting the methylene blue dye results in spillage of the contrast into the surgical field making procedure more messy. This can further complicate the surgery, which already has been made difficult due to previous recurrent surgeries and infections. Instead it is better to cannulate and palpate the fistulous tract, staying close to it while dissecting it and reaching up to the internal opening. It is also important to cover the suture line with the surrounding tissues to give a layered closure, so as to reduce the risk of recurrence. It is recommended to do a hemithyroidectomy, to reduce the risk of recurrence, if there are features of suppurative thyroiditis.7 Additionally, a period of nasogastric feeding further aids in healing.
CONCLUSION
Pyriform sinus fistulae are rare and require a high degree of suspicion and patience to delineate the fistula tract. A complete excision and layered closure of the opening in the pyriform sinus is mandatory to prevent recurrence.
REFERENCES
1. Schroeder JW, Mohyuddin N, Maddalozzo J. Branchial anomalies in the pediatric populationOtolaryngol Head Neck Surg 2008;137:289–295. DOI: 10.1016/j.otohns.2007.03.009
2. Madana J, Yolmo D, Kalaiarasi R, et al.Recurrent neck infection with branchial arch fistula in children. Int J of Pediatric 2011;75:1181–1185. DOI: 10.1016/j.ijporl.2011.06.016
3. Li W, Xu H, Zhao L, et al. Branchial anomalies in children: A report of 105 surgical cases. Int J Pediatr Otorhinolaryngol 2018;104:14–18. DOI: 10.1016/j.ijporl.2017.10.035
4. Nicoucar K, Giger R, Jaecklin T, et al.Management of congenital third branchial arch anomalies: a systematic reviewOtolaryngol Head Neck Surg 2012;142:21–28. DOI: 10.1016/j.otohns.2009.09.001
5. Nicoucar K, Giger R, Pope HG, Jr. et al.Management of congenital fourth branchial arch anomalies: a review and analysis of published casesJ Pediatr Surg 2009;44:1432–1439. DOI: 10.1016/j.jpedsurg.2008.12.001
6. James A, Stewart C, Warrick P, et al.Branchial sinus of the piriform fossa: reappraisal of third and fourth branchial anomalies. Laryngoscope 2007;117:1920–1924. DOI: 10.1097/mlg.0b013e31813437fc
7. Li Y, Lyu K, Wen Y, et al.Third or fourth branchial pouch sinus lesions: a case series and management algorithm. Journal of Otolaryngology- Head and Neck Surgery 2019;48:61. DOI: 10.1186/s40463-019-0371-6
8. Cha W, Cho SW, Hah JH, et al. Chemocauterization of the internal opening with trichloroacetic acid as first-line treatment for pyriform sinus fistula. Head Neck 2013;35(03):431–435. DOI: 10.1002/hed.22998
9. Huang YC, Peng SSF, Hsu WC. KTP laser assisted endoscopic tissue fibrin glue biocauterization for congenital pyriform fistula in children. Int J Pediatr Otorhinolaryngol 2016;85:115–119. DOI: 10.1016/j.ijporl.2016.03.028
10. Ishinaga H, Kobayashi M, Qtsu K, et al.Endoscopic electrocauterization of pyriform sinus fistula. Eur Arch Otorhinolaryngol 2017;274:3927–3931. DOI: 10.1007/s00405-017-4713-6
________________________
© The Author(s). 2021 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted use, distribution, and non-commercial reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.